Treatments
- Treatments
- Diagnostic Angiograms & Venograms
- Angioplasty & Stent Placement
- Aortic & Peripheral Stent-Grafts
- Transcatheter Embolization
- Transjugular Liver Biopsy
- TIPS (Transjugular Intrahepatic Porto-Systemic Stent Shunt)
- Intra-arterial & Venous Thrombolysis
- Inferior Vena Cava (IVC) Filter Placement
- Biliary Drainage Procedures
- Nephrostomy Tube & Nephroureteral Stent Placement
- Fallopian Tube Recanalization
- Musculoskeletal Embolization (Knee OA, Plantar Fasciitis)
- Prostatic Artery Embolisation
Biliary Drainage Procedures
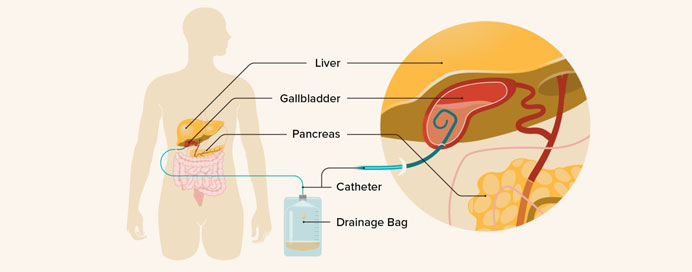
Biliary drainage procedures are minimally invasive interventions used to relieve obstruction in the bile ducts, which can occur due to stones, strictures, tumors, or post-surgical complications. Obstruction of bile flow can lead to jaundice, cholangitis, or liver dysfunction. The drainage can be performed percutaneously (through the skin) or endoscopically, depending on the patient’s condition and anatomy. Percutaneous transhepatic biliary drainage (PTBD) involves inserting a catheter directly into the bile ducts under imaging guidance to drain bile externally or internally into the intestine. Endoscopic biliary drainage, such as Endoscopic Retrograde Cholangiopancreatography (ERCP) with stent placement, allows internal drainage without external tubes. These procedures relieve symptoms, reduce infection risk, and improve liver function, often serving as a bridge to definitive treatment.
Indications
- Obstructive jaundice due to stones, strictures, or tumors
- Cholangitis (infection of bile ducts)
- Post-surgical biliary leaks or complications
Types of Biliary Drainage
- Percutaneous Transhepatic Biliary Drainage (PTBD)
- Catheter inserted through the liver into bile ducts
- Can be external (to collect bile outside the body) or internal (draining into intestine)
- Endoscopic Biliary Drainage (ERCP with stent)
- Endoscope used to place stent across obstruction
- Internal drainage into the intestine
Procedure Steps (PTBD example)
- Imaging guidance (ultrasound/fluoroscopy) used to locate bile duct
- Needle puncture into the bile duct through the liver
- Guidewire insertion followed by catheter placement
- Bile drained externally or connected to intestine
Benefits
- Relieves jaundice and symptoms
- Reduces risk of cholangitis
- Minimally invasive alternative to surgery
- Improves liver function before definitive treatment
Risks
- Bleeding at puncture site
- Infection or cholangitis
- Bile leak
- Catheter dislodgement or blockage
